
UC San Diego/N.C. A&T Bioengineering Pathways Program
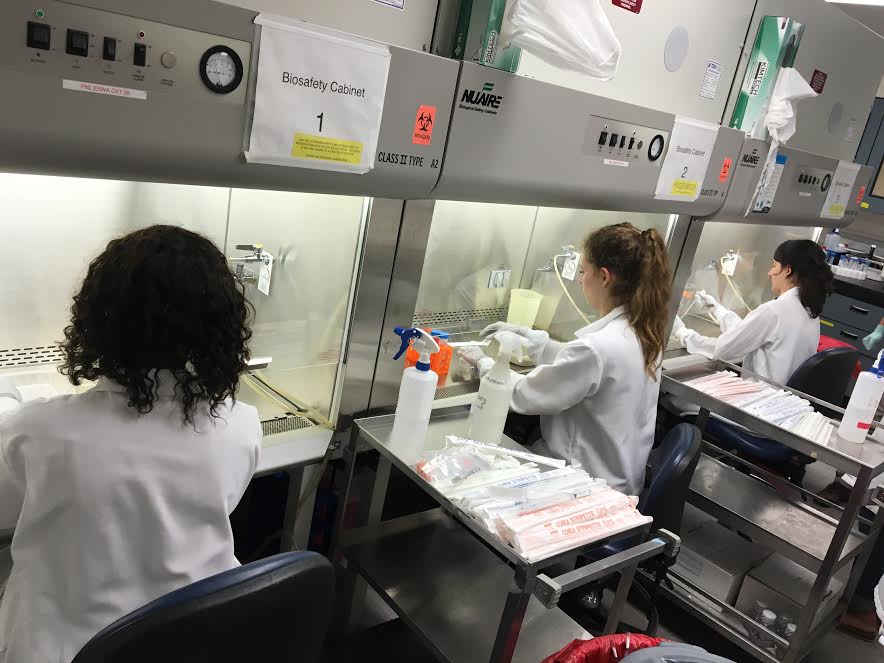
UC San Diego/N.C. A&T Bioengineering Pathways Program partnership is for undergraduates attending N.C. A&T. Funded by the UC Office of the President UC-HBCU Initiative, the eight-week program supports up to eight undergraduates from N.C. A&T each summer to engage in bioengineering research at UC San Diego. In addition to their significant research experience, participants will engage in professional development, networking, graduate preparation, and community-building activities. Program faculty mentors have expertise in bioengineering research and are highly supportive of engaging undergraduates in research.
About the Program
- Program Highlights
-
- Partnering with UCSD STARS: access to programming and logistical expertise
- $5,000 living allowance stipend, plus additional $1,120 food stipend
- Free on-campus housing
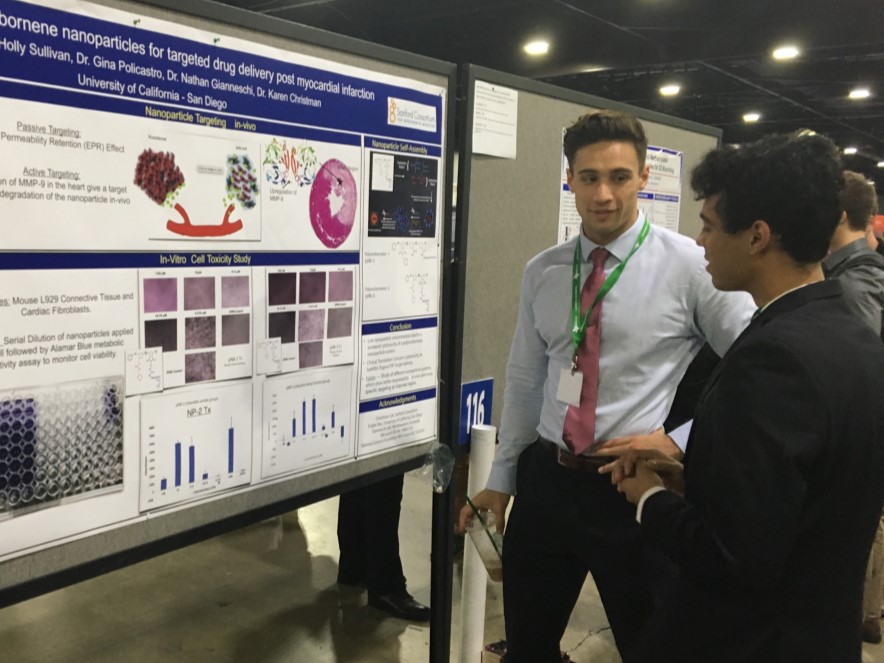
- Travel to and from San Diego and to the annual BMES Conference
- Presentation at UC San Diego Research Symposium
- Weekly research and professional skill development workshops
- Perform bioengineering research with program mentors
- Field trips and social events
- Eligibility Requirements
-
- Full-time undergrad student at N.C. A&T in relevant STEM degree program
- Participants must be 18+ years old by the start date of the program
- Currently a first-year, sophomore, or junior, with minimum G.P.A 3.0
- Full-time in-person availability during 8-week program: June 21 – August 14, 2026
This initiative is open to all eligible students and does not discriminate against, or grant preferential treatment to, any individual or group on the basis of race, color, national origin, religion, sex, disability, and/or other protected categories.
- Program Contacts
-
Dr. Alyssa C. Taylor, UCSD/N.C. A&T Bioengineering Pathways Program Director
- Application Information
-
- Major components of the application include:
- personal and academic information
- a personal statement
- a copy of your unofficial school transcript (as a pdf)
- letter of recommendation
- research faculty mentor preferences
- All components of the application must be submitted before the deadline to be considered complete.
- Only complete applications will be reviewed.
- Major components of the application include:
- Current Program Projects
-
The following descriptions provide examples of anticipated projects for the summer research mentors, so applicants can rank their preferences for research mentors based on research area. Details of specific projects will be finalized in conversations with research mentors nearer to the program’s summer commencement.Kolade Adebowale, Ph.D.
Assistant ProfessorUsing Viscoelasticity to Control Macrophage Functions in the Tumor Microenvironment
Tumor progression is strongly influenced by the mechanical properties of the extracellular matrix (ECM), which are altered by both intrinsic cellular remodeling and extrinsic factors such as diet-induced glycation. While increased ECM stiffness has been linked to enhanced tumor growth and metastasis, recent findings suggest that viscoelasticity—how tissues exhibit both solid-like and fluid-like behavior—offers a more accurate representation of the tumor microenvironment (TME).
Viscoelastic ECM properties not only promote cancer progression, such as in hepatocellular carcinoma (HCC) via the integrin-β1–tensin-1–YAP pathway, but also regulate immune cell behaviors. In particular, macrophages, which can infiltrate tumors and eliminate cancer cells, are influenced by ECM mechanics. However, current models fail to fully capture how viscoelasticity modulates macrophage function, limiting the development of effective macrophage-targeted therapies.
To address this gap, we will use our tunable viscoelasticity models—an in vitro alginate-collagen system and an in vivo diet-induced HCC mouse model—to test the hypothesis that macrophage behaviors are regulated by ECM viscoelasticity and in turn shape the tumor immune response. Our short-term goal is to validate our 3D culture system to study macrophage migration, phagocytosis, and tumor cell killing. Long-term, we aim to uncover viscoelasticity-driven mechanisms that can be leveraged for novel immunotherapeutic strategies.Brian Aguado, Ph.D.
Assistant ProfessorCardiovascular disease is the leading cause of death in both males and females, yet our mechanistic knowledge of the sex-specific molecular and cellular mechanisms that guide cardiovascular disease progression, particularly in females, remain poorly characterized. My laboratory uses precision biomaterials as in vitro and in vivo tools to dissect sex chromosome linked mechanisms that contribute to sex differences in cardiovascular diseases, specifically aortic valve stenosis and cardiac fibrosis. In my lab we use hydrogel biomaterials as engineered extracellular matrix mimics to explore sex dimorphisms in myofibroblast phenotypes in vitro and describe sex-specific molecular mechanisms that may drive dimorphisms in aortic valve stenosis and cardiac fibrosis. We also leverage animal models to decouple sex chromosomes from sex hormone effects on the inflammatory response to implanted biomaterials. Our work seeks to leverage biomaterial technologies to understand sex differences in health and disease, with the long-term goal of achieving sex and gender equity in cardiovascular disease treatments and outcomes.
Pedro Cabrales, Ph.D.
ProfessorWhole blood transfusion is a life-saving treatment
A newer option, low-titer group O whole blood (LTOWB), contains the right balance of red blood cells, plasma, and platelets, allowing it to be used in emergency situations for patients of any blood type. This summer project will explore strategies to improve the safety and effectiveness of LTOWB by studying a novel protein cocktail designed to detoxify hemoglobin breakdown products. Students will gain hands-on experience in blood biochemistry, vascular physiology, and transfusion medicine while contributing to a project with real-world medical applications.Fanny Chapelin, Ph.D.
Assistant ProfessorMR imaging of tumor associated macrophage changes with therapy
When functioning correctly, the immune system is a powerful force actively preventing disease and neoplastic development through immunosurveillance. Cancer cells evade the immune system through immunoediting, and begin recruiting anti-inflammatory macrophages, referred to as tumor-associated macrophages (TAM). TAM infiltration in tumors is an established biomarker of tumor aggressiveness and tumor resistance to therapy. Magnetic resonance imaging (MRI) based cell tracking techniques have proven successful in monitoring immune cell migration to the foci of inflammation in different pathologies, including cancer. This project will consist in developing MRI cell tracking methods for ex vivo and in situ labeling of cells with fluorine imaging reagents. We will develop non-invasive MRI imaging methods that could serve as a prognostic biomarkers of therapy efficacy or tumor recurrence. We will deliver fluorine nanoemulsions intravenously to mice bearing subcutaneous tumors. As a result, systemic monocytes, macrophages and TAM will be labeled, and we will quantify longitudinal MR signal changes following radiation therapy or programmed cell death protein-1 (PD-1) immunotherapy. Participating students will learn cell culture and labeling techniques for subsequent MR imaging of infused cells. The student will also learn about animal models and experimentation, specifically mouse handling and tumor injection. The REU student will receive training in MRI safety and accompany the PI during the MRI experiments.Erika Cyphert, Ph.D.
Assistant ProfessorEngineering mucoadhesive polymers to target microbiome communities
In this project we will engineer a mucoadhesive delivery platform for microbial-derived metabolites to allow for their sustained and controlled delivery to either the gut or vaginal mucosa to address antibiotic-resistant/recurrent infections. The design of the polymeric formulation will account for ease of administration (thermogelling - gel at body temperature at administered site), for targeted release (mucoadhesive - to prolong retention at target site), and degradation based upon the microenvironment conditions (pH-based stimulus for degradation/release). Students may also have the opportunity to work with mouse models and culture bacteria.Adam Engler, Ph.D.
ProfessorMaterial Cues Guide Metastatic Behavior
Common biological markers of metastasis have been difficult to identify, but all metastatic cells must detach from their tumor and migrate through the adjacent tissue to reach a blood vessel. We find that cells with weak adhesion to their surrounding tissue are the most aggressive and form tumors at higher rates. The Participant will use a new cell separation technology with varied adhesive biomaterial substrates to assess which materials best separate metastatic cells based on adhesive differences and the Participant will then measure their invasive capacity in vitro. This work compliments boarder efforts to develop diagnostic assays that use adhesion to understand how tumor cells migrate.Prashant Mail, Ph.D.
ProfessorGene and Cell Therapy
The major research thrusts in the Mali laboratory are two-fold: one, development of molecular toolsets for genome, transcriptome, and proteome engineering and their application to systematic genome interpretation and gene therapy applications; and two, study and engineering of cell fate specification during development utilizing human pluripotent stem cells as the core model system. Given the parallels in phenotypes (such as self-renewal and tumor forming ability) between pluripotent stem cells and cancer cells, a key research thrust is also in dissecting aberrant cellular transformation processes such as during tumorigenesis. One example hypothesis: the student participant will test the hypothesis that misregulation of developmental genes in adulthood has the potential to drive tumorigenesis.Ester Kwon, Ph.D.
Associate ProfessorTraumatic brain injury affects millions of Americans every year, yet there are no therapeutics that can address the long-term impairments that the majority of survivors will experience.
The Kwon lab develops nanoscale technologies to measure proteolytic activity and deliver therapeutic molecules in the context of the injured brain. Nanomaterials - materials are on the length scale of 10-100 nanomaters - can have unique access to the brain microenvironment based on their small size and be programmed with multiple functions. The student will learn how to synthesize and characterize nanomaterials and evaluate them in a biological context, either in cell culture or in mouse models of traumatic brain injury in close collaboration with members in the lab.Andrew McCulloch, Ph.D.
ProfessorStudies of elite human performance in athletes using biomechanics, imaging and data science.
Good for a student interested in sports and with some experience in Python programming.Robert Sah, Ph.D.
ProfessorBioengineering the knee.
Our knees are amazing biomechanical and mechanobiological structures! They normally support large loads and facilitate motion with little friction or wear. They adapt to mechanical demands during growth and in adulthood. However injury and aging often lead to debilitating knee osteoarthritis. Bioengineering large osteochondral grafts is poised to transform the field of orthopedic surgery from the 20th century of "Prosthetic Joint Replacement" to 21st century "Biological Joint Resurfacing". Our continuing studies (A) develop bioengineering technologies in biomechanics, mechanobiology, bioimaging, and bioreactor, to (B) better understand the knee in growth, health, and deterioration, relating composition, structure, function, and metabolism, and to (C) develop tissue engineering and regenerative medicine therapies for knees. Depending on their background and interests, summer students can focus on a (A) bioengineering method, (B) scientific question, and/or (C) diagnostic or therapeutic application.Lingyan Shi, Ph.D.
Associate ProfessorUsing stimulated Raman scattering to Understand Cell Mechanics
The Shi lab is developing novel multimodal optical imaging platforms integrating stimulated Raman scattering (SRS), multiphoton fluorescence (MPF), and second harmonic generation (SHG) for visualizing metabolic dynamics in cells and tissues and their impact on tissue mechanics. The participant will learn how to use these cutting-edge state-of-the-art high resolution imaging technologies and code custom designed algorithms for imaging analysis. These methods will be applied to heart tissues undergoing stretch, which will provide training in the use of powerful tools for disease detection, diagnosis, and prognosis.Daniela Valdez-Jasso, Ph.D.
Associate ProfessorMechanics of Pulmonary Arterial Hypertension (PAH)
PAH is a rapid, progressive vascular disease that commonly results in intractable right-heart failure and premature death. To better understand the remodeling process undergone by the pulmonary arteries, the participant will characterize the time course of the pulmonary vascular changes that occur in pulmonary vessels and the relation of these changes to cardiac mechanics. To this end, the participant will mechanically stimulate cells derived from pulmonary arteries and right ventricles from control animals to mimic in vivo conditions and compare them to cell phenotypes from hypertensive animals. - Proposition 209 Compliance
-
In accordance with applicable Federal and State law and University policy, the University of California does not discriminate, or grant preferences, on the basis of race, color, national origin, religion, sex, disability, and/or other protected categories.
More information about Proposition 209 can be found here.
More information about the University of California Anti-Discrimination Policy can be found here.
Initiatives are open to all eligible members of the UC San Diego campus community and does not discriminate against, or grant preferential treatment to, any individual or group on the basis of race, color, national origin, religion, sex, disability, and/or other protected categories.
Applications for summer 2026 are now closed.
We will notify all applicants of the outcome via email by March 9th 2026.
For any questions, please contact:
Dr. Alyssa C. Taylor, UCSD/N.C. A&T Bioengineering Pathways Program Director, atayloramos@ucsd.edu
